Fixed Packaging of Alzheimer’s Drug May Waste $605 Million a Year for Medicare, Experts Warn
Controversial drug comes in fixed-dose vials, with excess discarded after each useMedicare could potentially waste up to $605 million annually from the packaging of controversial Alzheimer’s drug aducanumab if it is approved for widespread use, according to a University of California Los Angeles (UCLA) study. “Given Medicare’s premium increase in 2022 partly due to aducanumab, greater focus on efficient vial packaging could improve the value of future Medicare spending, slow premium growth, and reduce beneficiaries’ out‐of‐pocket costs,” said Dr. Carlos Irwin Oronce in the study’s media release. To reduce wastage, the authors proposed flexible packaging rather than vials set at fixed dosages. Since the drug is fixed in its dosage volume and given to patients based on their weight, what remains after it is administered is discarded, resulting in waste. With 2.9 million to 8.4 million Medicare beneficiaries eligible for the drug, if approved for widespread use, Medicare could be wasting around $115 million to $605 million per year even if only 10 percent of those eligible choose the prescription. The Centers for Medicaid and Medicare (CMS) announced in April 2022 that the drug can only be accessed under Medicare through clinical trials. However, this decision may be overturned if Biogen—the manufacturer of aducanumab—sues CMS for this decision, likely leading to widespread approval, according to the authors. The drug currently comes in fixed-dose vial sizes of 170 mg per 1.7 ml and 300 mg per 3.0 ml. It is administered monthly at an average dose of 10 mg per kilogram for each patient. The authors calculated around $2,300 in waste value every month for each patient. Controversial Alzheimer’s Disease Medication Despite being the only drug approved by the Food and Drug Administration (FDA) for treating Alzheimer’s, medical experts are highly dubious of the drug’s efficacy. Many health care facilities announced that they will not provide aducanumab for their patients out of concern for the drug’s effectiveness and safety. The drug is marketed as aduhelm for patients with mild cognitive impairment, meaning a mild decrease in memory and or thinking but not yet affecting the functioning state. Aducanumab reduces protein plaques in the brain, often implicated in the death of nerves and a hallmark of Alzheimer’s disease. Nonetheless, scientists are still unclear whether these protein plaques cause memory loss or Alzheimer’s disease. This becomes concerning when Biogen’s clinical trials also showed no evidence that the drug improves cognition. Two trials testing efficacy were stopped in 2019 because there was no clinical benefit shown. The company later reviewed the data and found a small improvement in symptoms in one group of patients, prompting Biogen’s application with the FDA (pdf). Aducanumab has been found to increase the risk of brain bleeds and swelling. UCLA estimated in January 2022 that ancillary care services such as MRI and neurologist visits to monitor these drug-associated potential adverse effects may account for nearly 20 percent of the total Medicare costs related to the drug, or over $6,500 per patient per year. Aducanumab was approved by the FDA through an accelerated approval pathway on June 7, 2021. Biogen originally priced the drug at $56,000 per year per patient and later halved the costs to $28,200 in December 2021 after facing widespread criticism.
Controversial drug comes in fixed-dose vials, with excess discarded after each use
Medicare could potentially waste up to $605 million annually from the packaging of controversial Alzheimer’s drug aducanumab if it is approved for widespread use, according to a University of California Los Angeles (UCLA) study.
“Given Medicare’s premium increase in 2022 partly due to aducanumab, greater focus on efficient vial packaging could improve the value of future Medicare spending, slow premium growth, and reduce beneficiaries’ out‐of‐pocket costs,” said Dr. Carlos Irwin Oronce in the study’s media release.
To reduce wastage, the authors proposed flexible packaging rather than vials set at fixed dosages. Since the drug is fixed in its dosage volume and given to patients based on their weight, what remains after it is administered is discarded, resulting in waste.
With 2.9 million to 8.4 million Medicare beneficiaries eligible for the drug, if approved for widespread use, Medicare could be wasting around $115 million to $605 million per year even if only 10 percent of those eligible choose the prescription.
The Centers for Medicaid and Medicare (CMS) announced in April 2022 that the drug can only be accessed under Medicare through clinical trials.
However, this decision may be overturned if Biogen—the manufacturer of aducanumab—sues CMS for this decision, likely leading to widespread approval, according to the authors.
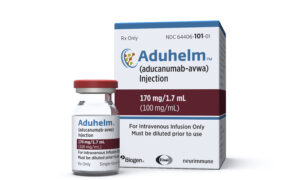
The drug currently comes in fixed-dose vial sizes of 170 mg per 1.7 ml and 300 mg per 3.0 ml. It is administered monthly at an average dose of 10 mg per kilogram for each patient.
The authors calculated around $2,300 in waste value every month for each patient.
Controversial Alzheimer’s Disease Medication
Despite being the only drug approved by the Food and Drug Administration (FDA) for treating Alzheimer’s, medical experts are highly dubious of the drug’s efficacy.
Many health care facilities announced that they will not provide aducanumab for their patients out of concern for the drug’s effectiveness and safety.
The drug is marketed as aduhelm for patients with mild cognitive impairment, meaning a mild decrease in memory and or thinking but not yet affecting the functioning state. Aducanumab reduces protein plaques in the brain, often implicated in the death of nerves and a hallmark of Alzheimer’s disease.
Nonetheless, scientists are still unclear whether these protein plaques cause memory loss or Alzheimer’s disease. This becomes concerning when Biogen’s clinical trials also showed no evidence that the drug improves cognition.
Two trials testing efficacy were stopped in 2019 because there was no clinical benefit shown. The company later reviewed the data and found a small improvement in symptoms in one group of patients, prompting Biogen’s application with the FDA (pdf).
Aducanumab has been found to increase the risk of brain bleeds and swelling.
UCLA estimated in January 2022 that ancillary care services such as MRI and neurologist visits to monitor these drug-associated potential adverse effects may account for nearly 20 percent of the total Medicare costs related to the drug, or over $6,500 per patient per year.
Aducanumab was approved by the FDA through an accelerated approval pathway on June 7, 2021.
Biogen originally priced the drug at $56,000 per year per patient and later halved the costs to $28,200 in December 2021 after facing widespread criticism.












